Podcast: Play in new window | Download (Duration: 45:09 — 83.0MB)
Babies need the proper bacteria to enhance growth, development and immunity

Infants are bathed in protective, beneficial microflora as they pass through their mother’s birth canal. As a result, babies delivered vaginally are bathed with friendly, protective Bifido bacteria. In contrast, babies delivered by caesarian section (C-section) become bathed in the bacteria from their environment–most often, they’re exposed to the bacteria on the skin of their mother and the bacteria in the hospital delivery room. When this occurs, babies lose out on the benefits that B. infantis supplies. They miss the natural boost to their defenses, and don’t receive the digestive support for their inexperienced gastrointestinal tract–not the best start to lifelong health.
Breastfeeding by a healthy mother further enriches an infant’s protective microflora and enhances an infant’s growth and development. For example, probiotic microorganisms set up attachment sites on the infant gastrointestinal (GI) wall to form a microbial barrier that protects against invasion from less desirable and potentially harmful microorganisms. B. infantis is a natural inhabitant of the intestines in human infants and also occurs in small numbers in the human vagina. In addition, it is one of the predominant bacteria in the infant’s large intestine along with other Bifidobacteria species such as B. bifidum, B. longum, and B. breve.
 Human breast milk evolved for three purposes:
Human breast milk evolved for three purposes:
- Supply the nutritional needs of the infant;
- Expose the infant to maternal immune properties;
- Shape the infant gut microbiota.
Breast milk is a fluid synthesized at the mother’s expense and shaped throughout evolution to nourish the infant and improve its rate of survival. Breast milk provides many benefits for the infant. For example, not only is breast milk the best food for the infant, but it also provides human milk oligosaccharides that stimulate Bifidobacterium infantis.
Many studies show that Bifidobacterium is a dominant genus in the intestinal microbiota of breast-fed infants. In some cases, Bifidobacterium takes up approximately 75% of total bacteria. The representation of Bifidobacterium is less observed in formula-fed infants, who have more of a diverse microbiota. The difference in bacterial colonization between breast-fed and formula-fed infants can be explained in great part by the non-essential components in human milk. The predominance of Bifidobacterium in breast-fed infants was first noticed over 100 years ago. It suggested that breast milk contained certain molecules that stimulated the growth of these bacteria, defined as Bifidus factors. In a 1980 German study, B. infantis was the predominant beneficial bacteria found in infants.
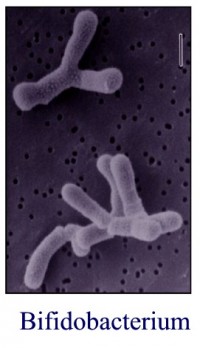 Alarmingly, since that time, researchers have found a decline in the numbers of B. infantis found in infants, including breast-fed infants. The difference of the microbiota of breast-fed healthy infants is demonstrated for its specific selection of B. infantis species and also to some extent B. bifidum. Basically, it appears that by the process of evolution and selection, breast-milk components favor the growth of B. infantis. Therefore, we should mimic what evolution has taught us and supplement with only B. infantis to enhance the infant gut microbiota.
Alarmingly, since that time, researchers have found a decline in the numbers of B. infantis found in infants, including breast-fed infants. The difference of the microbiota of breast-fed healthy infants is demonstrated for its specific selection of B. infantis species and also to some extent B. bifidum. Basically, it appears that by the process of evolution and selection, breast-milk components favor the growth of B. infantis. Therefore, we should mimic what evolution has taught us and supplement with only B. infantis to enhance the infant gut microbiota.
Bifidobacteria, including B. infantis, have the following characteristics:
- Anaerobic bacteria (does not require oxygen for growth).
- Produce acetic and lactic acids, and small amounts of formic acid, from carbohydrates. These organic acids increase the acidity of the intestines and thereby inhibit undesirable bacteria.
- Optimum growth occurs at 98-105o F.
- Prevent the colonization of the intestines by pathogens by competing for nutrient and attachment sites.
- Assist nitrogen retention and weight gain in infants.
- Inhibit bacteria that convert nitrates to potentially harmful nitrites.
- Produce vitamins in the B-complex family.
As reported, Bifidobacteria and the specific substances they secrete can protect the intestinal mucosa in infants. When the microflora of infants becomes disturbed from oral antibiotic therapy, vaccinations, convalescences or sudden weather changes, the levels of Bifidobacteria decline and lead to lower levels of digestive health. The use of a Bifidobacterium infantis NLS supplement can help with the nutritional restoration of the intestinal microflora. (The above information is excerpted from Life Start brochure by Natren.)
 Here is a recent study reported on PubMed entitled “Bifidobacterium longum subspecies infantis: champion colonizer of the infant gut” CLICK HERE to read more.
Here is a recent study reported on PubMed entitled “Bifidobacterium longum subspecies infantis: champion colonizer of the infant gut” CLICK HERE to read more.
About Natasha Trenev
Probiotic pioneer Natasha Trenev has been committed to formulating and manufacturing probiotics of unparalleled quality for 30 years. Natren has willingly subjected itself to the most stringent international manufacturing quality control process, undergoing extensive testing from raw materials to finished probiotic products. The Trenev Process® uses a unique process to substantially increase the probiotic activity, while eliminating the need for additives. To listen to my previous interview with Natasha: CLICK HERE.










{ 0 comments… add one now }